July 17, 2025
Psychiatry insurance transition timeline guide

Written by
Osmind
Start taking insurance with confidence. Learn the essential timeline, documentation, and partner selection strategies that set successful psychiatry practices up for insurance success.
The decision to take insurance may seem daunting, but with proper planning and the right partner, it's one of the most rewarding decisions you can make for your practice.
The payoff is significant: expanded patient access, predictable revenue streams, reliably offering breakthrough treatments like Spravato and TMS, and the ability to help patients who couldn't afford private pay rates. But success depends on understanding the process upfront and preparing accordingly.
This guide covers the timeline and essential documents you need to avoid costly mistakes and set yourself up for smooth sailing. You'll learn:
- The realistic timeline for transitioning from private pay to insurance
- Essential documentation that accelerates the approval process
- Why the right billing partner makes all the difference
- Smart patient communication strategies that build trust
- Special considerations for TMS and Spravato practices
- How to choose the ideal billing partner for psychiatry
Pro tip: If you're feeling overwhelmed by the insurance process, Osmind is your complete practice operations partner. Our team let's you focus on patient care while we handle psychiatry billing and practice management—everything from credentialing, payer enrollment and ongoing maintenence, and RCM, often reducing your time-to-revenue by 30-60 days and increasing your net collections rate.
How long does it take to get up and running with insurance and seeing patients?
"I want to start taking insurance in two months."
This timeline reflects enthusiasm and urgency—both good things. But successful practices understand that insurance acceptance is a process, not a single decision.
Here's what typically happens. A practice decides to expand their patient base by taking insurance. They pick a target date—usually 8-10 weeks out—and try to make everything fit that timeline. But you're not just dealing with your own schedule; you're dependent on payer approval processes, background checks, and committee meetings that happen on schedules you can't control.
When reality hits, they're scrambling to reschedule patients, explain delays, and manage the fallout from unrealistic expectations.
The reality check: Most practices think the process takes 2 months. Plan for 4-6 months minimum.
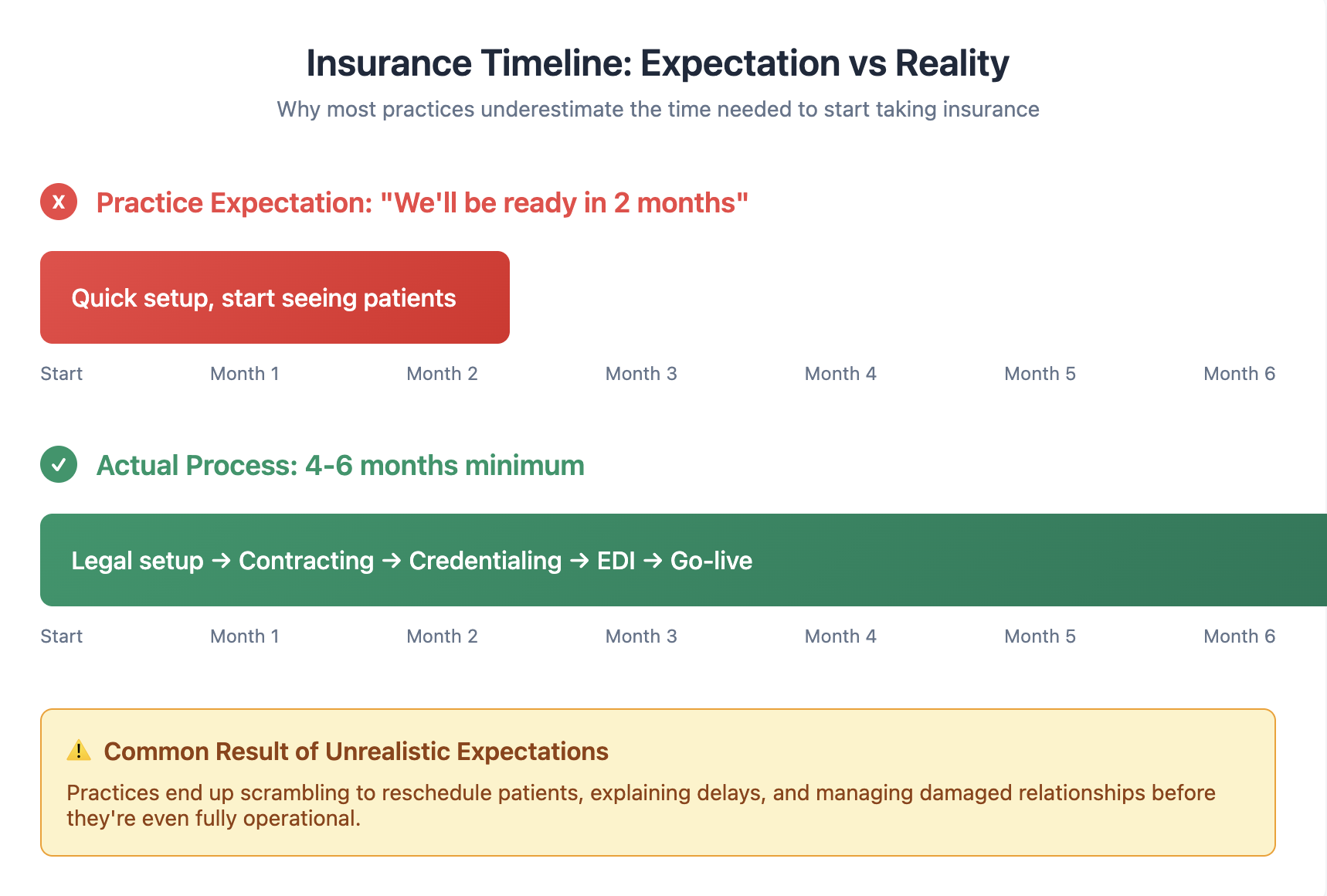
Smart preparation creates competitive advantages: smooth revenue transition during the approval process, strong patient relationships through clear communication, higher claim approval rates due to proper setup, confident staff who understand the new processes, and enhanced practice reputation as a trusted insurance provider.
The Dependency Chain That Trips Everyone Up
Taking insurance isn't a single process—it's a rigid sequence where each step requires completion of the previous one. You can't skip steps or run them simultaneously.
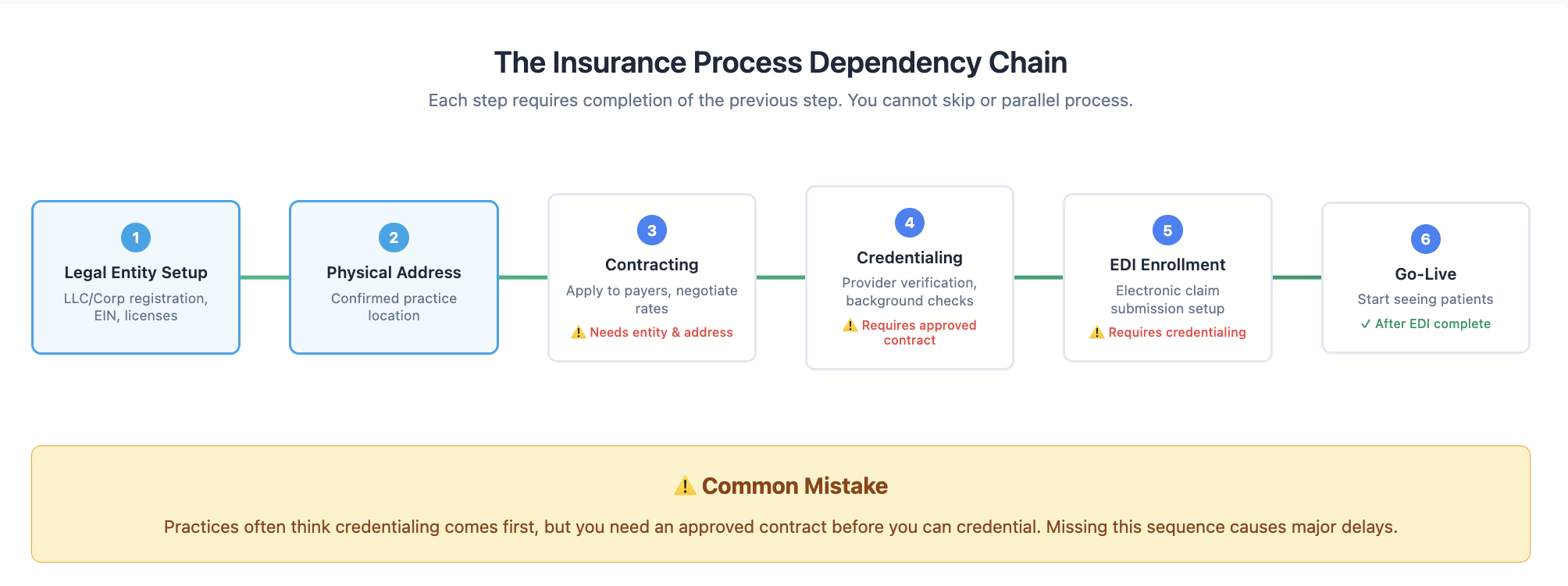
The most common failure point? Practices think credentialing comes first, but you actually need an approved contract before you can credentialied. Then, even after credentialing is complete, you still need EDI enrollment before you can start seeing patients. Each step has dependencies that you need to anticipate.
For a detailed walkthrough of the credentialing process, including step-by-step instructions and timeline management, see our guide: Insurance Credentialing Guide for Mental Health Clinicians.
Essential Documentation for Success
Now that you understand the timeline, you need to get your documents in place. Having complete documentation ready accelerates every step of the credentialing process.
Core business documentation:
- Legal business entity documentation
- NPI number (individual and group)
- W-9 tax form
- Void check or bank letter
- Practice location details and hours of operation
- Current malpractice coverage
- Updated CAQH profile
Each clinician needs:
- Current medical licenses
- DEA registration
- Board certifications
- Professional references
- Complete CVs with at least five years of work history
Business setup requirements:
- Taxonomy codes (especially critical for TMS/Spravato)
- Target insurance plans list
- Benefit type research (medical vs. behavioral vs. pharmacy)
The CAQH profile deserves special attention since most insurers use this platform for provider verification. Set up your profile early, submit all supporting documents, and remember that you'll need to attest quarterly to keep it current. Delays in CAQH maintenance are a common cause of credentialing holdups.
Choosing Your Ideal Billing Partner
With proper documentation and realistic timelines in place, your success depends on choosing a billing partner who truly understands psychiatry's unique requirements.
Psychiatric practices face billing challenges that general medical billing services can't handle—from mental health parity laws to complex prior authorizations for interventional treatments. Specialized partners deliver 95%+ collection rates compared to 85% with general billers, while saving you 20+ hours monthly on administrative tasks.
For comprehensive guidance on evaluating billing services, including detailed checklists and red flags to avoid, see our complete guide: How to Choose the Right Psychiatric Billing Service for Your Practice.
Ready to expand your practice with confidence? Osmind is your complete practice partner. We provide comprehensive EHR, credentialing, and billing services specifically designed for forward-thinking psychiatry practices. Our team handles the entire process, so you can focus on patient care.
Learn more about Osmind's all-in-one EHR, credentialing, and billing solution
Special Considerations for Interventional Practices
If you're planning to offer TMS or Spravato, your situation becomes more complex. Interventional treatments require specific training and practice certification to perform, and they aren't always covered under the same insurance benefit.
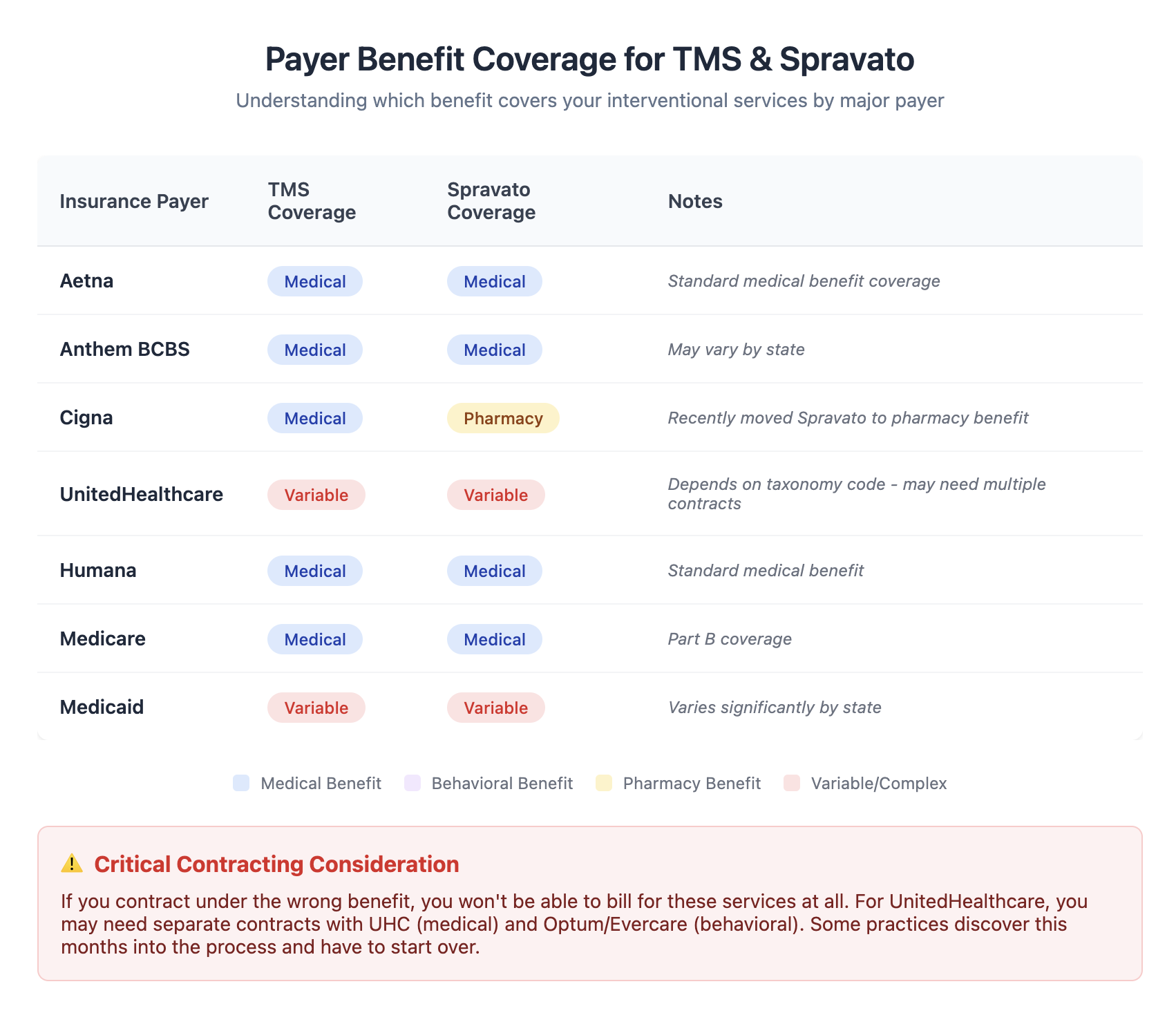
You need to understand which benefit covers your services for each payer before you apply. Contract under the wrong benefit, and you won't be able to bill for these services at all.
The landscape varies dramatically by payer. Most cover Spravato under the medical benefit, but UnitedHealthcare varies based on your taxonomy code, and Cigna recently moved to pharmacy benefit only. For UnitedHealthcare, you might need separate contracts—one with UHC for medical services and another with Optum/Evercare for behavioral services. This isn't just checking a different box; it's literally two different applications with separate approval processes.
Osmind navigates these payer-specific requirements for you, ensuring you get the right contracts for all your services.
The Critical Patient Communication Rule
Don't schedule patients until EDI enrollment is complete.
This is the golden rule that prevents the most common disaster: having to reschedule patients due to approval delays. "You really don't want to have to reschedule patients," as one practice manager told us after learning this lesson the hard way. When you're forced to reschedule, you're damaging trust before your practice is even fully operational.
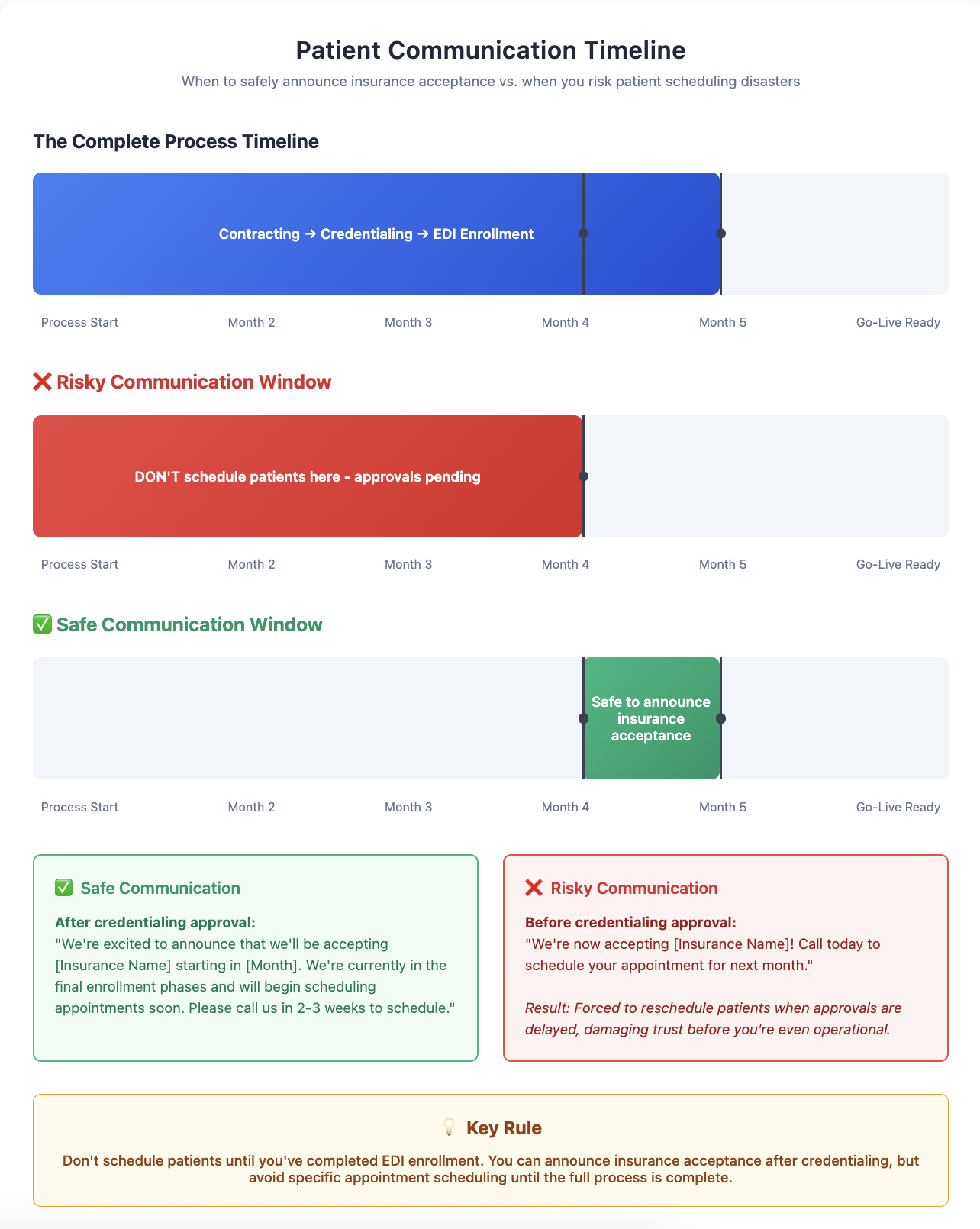
You can announce you're accepting insurance after credentialing approval, but avoid scheduling specific appointments until the full process is complete. The safe communication window shows exactly when to make different types of announcements without risking patient relationships. Work backwards from a realistic timeline to determine when you can safely communicate with patients about insurance acceptance.
The Staff Training Problem Nobody Talks About
Even with perfect preparation, your staff's execution can sabotage your billing success. "The number one reason for claim rejections and denials is the wrong insurance was entered." This isn't a billing service problem—it's a front desk training problem.
Here's how complex insurance selection gets: A patient lives in Oregon but has Anthem coverage, which is actually a California Blue Cross plan. Your staff shouldn't register them under "Anthem"—they should register them under their local Oregon Blue Cross plan. How is your front desk supposed to know this? Usually, they learn through expensive trial and error.
The best billing services provide ongoing staff training and build guardrails into their systems to prevent these errors. When evaluating partners, prioritize those who work directly with your front desk staff, not just providers or practice managers.
Osmind includes built-in insurance selection guardrails and ongoing staff training to prevent these costly errors before they happen.
Moving Forward with Confidence
Taking insurance is complex, but it's predictable. The timeline is longer than you'd prefer, but the documentation requirements are clearly defined. Success depends on realistic timeline planning, thorough preparation, and choosing an expert partner who understands psychiatry.
The right billing partner will provide realistic timelines with clear dependencies, handle psychiatry-specific requirements proactively, train your staff to prevent common errors, and communicate clearly throughout the process.
Ready to simplify your insurance journey? Osmind is your complete practice partner. We provide comprehensive EHR and billing services specifically designed for forward-thinking psychiatry practices. Our specialized team handles the entire process, so you can focus on patient care instead of bureaucracy.
Learn more about Osmind's all-in-one EHR and billing solution
Connect with forward-thinking peers, advance your practice, and attend expert events. Join the Psychiatry Collective today.







.png)

